Prediabetes & Diabetes
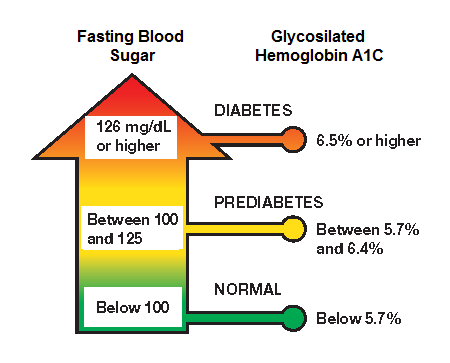
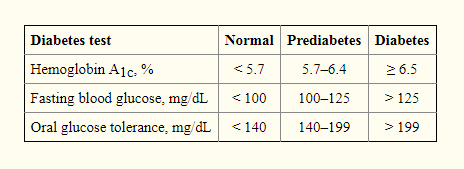
/Diagnosis of diabetes is determined by a fasting plasma glucose (FPG) test (>126 mg/dL, or a glycated hemoglobin (HbA1c) test (>6.5%)
In prediabetes, blood sugar levels are higher than normal but not high enough to be diagnosed as type 2 diabetes. The diagnostic criteria for prediabetes are FPG levels of 100–125 mg/dL, or a HbA1c of 5.7% to 6.4%.
According to the Centers for Disease Control and Prevention (CDC), people most at risk for prediabetes are overweight, age 45 or older, have a family history of type 2 diabetes, participate in physical activity fewer than three times a week, had gestational diabetes, and/or have polycystic ovary syndrome.
Many people with prediabetes who ignore lifestyle modifications will develop type 2 diabetes within five years.
In addition, a person with undiagnosed or untreated prediabetes is also at increased risk for heart disease and stroke due to the degenerative changes that occur when blood glucose levels are poorly controlled.
Microangiopathy, in which the capillary basement membrane becomes thick and hard, causes obstruction or rupture of capillaries and small arteries, resulting in tissue necrosis and loss of function, as in the case of a myocardial infarct or cerebrovascular accident.
Vascular degeneration in the kidney glomeruli—diabetic nephropathy—eventually leads to chronic renal failure.
Of the 2011 to 2014 population of adults with prediabetes, 36.6% had hypertension, 51.2% had dyslipidemia, 24.3% smoked, 7% had albuminuria, 4.6% had reduced estimated glomerular filtration rate, and a 10-year cardiovascular event risk ranged from 5% to 7%.
For overweight or obese adults ages 40 to 70, the US Preventive Services Task Force (USPSTF) recommends screening for abnormal blood glucose as part of a cardiovascular risk assessment.
Results from the US Diabetes Prevention Program (DPP)—a randomized clinical study of more than 3,000 nondiabetic subjects with elevated fasting and postload plasma glucose concentrations—demonstrated that lifestyle intervention reduced diabetes incidence by 58%, whereas the prescription drug metformin reduced it by 31% compared with a placebo.
Intensive lifestyle intervention with diet and physical activity, have long-term beneficial changes and reduced diabetes risk. The incidence of converting from prediabetes to diabetes was approximately 2% for those who lost at least 5% of their body weight vs about 8% for those who gained more than 2.5% of their body weight.